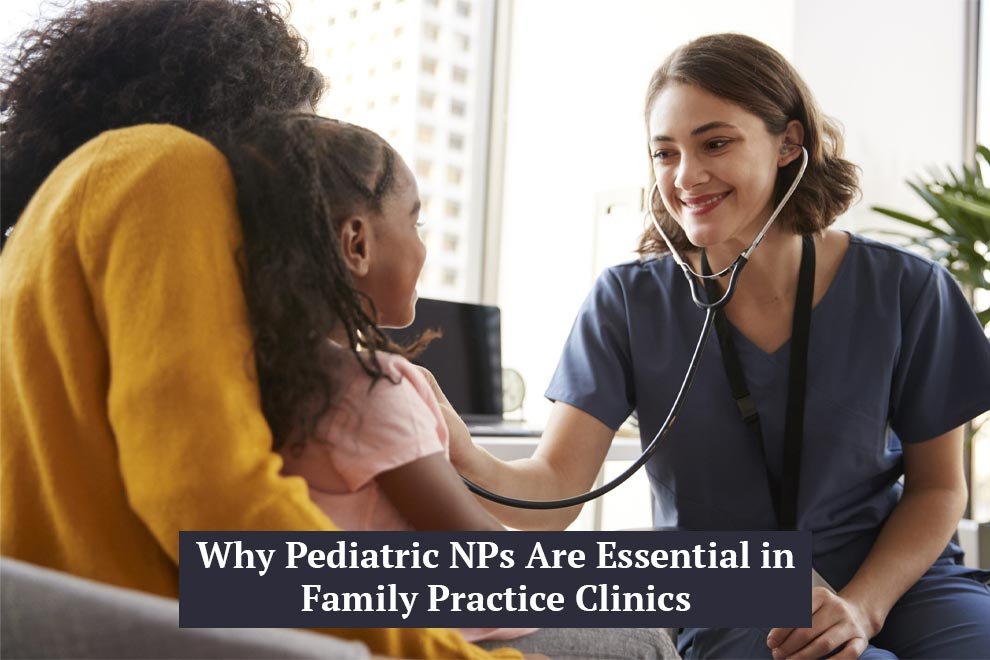
The landscape of family healthcare is changing rapidly, and Pediatric Nurse Practitioners (PNPs) are playing a pivotal role in this transformation. As the demand for primary care services grows, particularly for pediatric populations, PNPs are stepping up to provide high-quality, specialized care that complements the work of family physicians. Their extensive training in pediatric health and development allows them to focus on the specific medical and emotional needs of children within the broader family unit.
Family practice clinics, traditionally designed to care for individuals across all life stages, benefit immensely from the inclusion of PNPs. These practitioners bring a level of depth and precision to pediatric care that ensures children are not only treated appropriately but are also monitored with a developmental lens. Whether managing routine wellness checks, identifying early behavioral concerns, or providing immunizations, PNPs offer a level of attentiveness that aligns closely with best practices in child healthcare.
Beyond clinical expertise, PNPs often serve as advocates for pediatric patients within the family care setting. They educate caregivers, counsel on preventive health strategies, and build relationships that foster long-term trust. Their holistic, family-centered approach makes them uniquely equipped to understand and manage the complex dynamics involved in caring for children as part of a family system. In this way, PNPs are not merely healthcare providers; they are vital partners in family health and wellness.
Bridging the Pediatric Care Gap in Family Settings
In many communities, particularly those that are rural or underserved, access to pediatric-specific medical care can be inconsistent or altogether absent. Family practice clinics that integrate PNPs into their care teams help bridge this critical gap. The presence of a pediatric specialist within a general care setting eliminates the need for families to travel long distances or navigate complicated referral systems just to get their child seen by someone with pediatric expertise.
These clinics benefit from the continuity and convenience that a PNP brings to pediatric care. Rather than referring patients out for issues that require specialized attention, a PNP can address concerns ranging from developmental delays to adolescent health matters directly within the clinic. This not only enhances the quality of care but also strengthens the bond between healthcare provider and patient, which is a cornerstone of effective family medicine.
A comprehensive understanding of how PNPs support the flow of care within family clinics is illustrated by the structured, team-based approach often described in models like those used by Collaborating Docs. These frameworks emphasize how PNPs handle a broad spectrum of pediatric responsibilities, from routine checkups to managing long-term developmental conditions, as part of the clinic’s integrated care strategy. This continuous engagement enables clinics to respond efficiently to the evolving needs of young patients while maintaining a consistent, high standard of care.
Enhancing Preventive Care and Early Intervention
Preventive care remains one of the most effective strategies for promoting long-term health, particularly in pediatric populations. Pediatric Nurse Practitioners are highly trained in identifying early signs of illness, developmental issues, and risk factors that might otherwise go unnoticed in a busy general practice. Their role in early intervention is critical, not just for addressing current health concerns but for laying the groundwork for a healthier adulthood.
Well-child visits, for instance, are a routine yet vital component of pediatric care. PNPs use these appointments to track growth metrics, assess developmental milestones, and engage parents in discussions about nutrition, sleep, and behavior. These interactions serve not just as medical checkups, but as valuable educational moments that help parents make informed choices about their child’s well-being. Early detection of physical or emotional issues during these visits can lead to timely referrals or interventions that alter a child’s health trajectory for the better.
In family practice settings, where practitioners often juggle patients across the lifespan, having a PNP focus solely on pediatric preventive care strengthens the clinic’s overall care model. Their specific training enables them to distinguish between what is typical and what may require further evaluation. This sharp clinical instinct, combined with their approachable style of communication, makes PNPs indispensable in driving health outcomes that start early and last a lifetime.
Collaborative Practice and Team Integration
One of the most defining strengths of a Pediatric Nurse Practitioner is their ability to function seamlessly within a multidisciplinary healthcare team. Family practice clinics often operate as collaborative environments, and the inclusion of a PNP adds both balance and depth to the team structure. Their insights into child health provide a valuable complement to the broader skill sets of physicians, nurses, and allied health professionals.
In many cases, PNPs take the lead in managing pediatric cases while coordinating care with other specialists when necessary. This teamwork approach is crucial for children with chronic illnesses or complex needs that require input from various healthcare disciplines. PNPs help to ensure that care plans are not only medically sound but also coherent and understandable to families, reducing confusion and increasing adherence to treatment recommendations.
Their integration into the team also allows for more efficient use of clinic resources. With a PNP managing pediatric care, physicians can focus on adult or geriatric patients without compromising the quality of care for children. This balance leads to shorter wait times, better access, and a more patient-centered experience across the board. As collaborative care continues to define modern family medicine, PNPs are proving to be irreplaceable contributors to that model.
Addressing Behavioral and Mental Health Challenges
Behavioral and mental health concerns among children and adolescents have become more visible in recent years, prompting a shift in how primary care providers approach pediatric care. Pediatric Nurse Practitioners are particularly well-equipped to recognize and manage these challenges within the family practice setting. Their routine interactions with children allow them to observe behavioral patterns and emotional cues that may indicate deeper concerns.
In addition to standard developmental assessments, PNPs often conduct screenings for anxiety, depression, ADHD, and other common childhood mental health issues. These screenings are embedded into regular wellness visits, making it easier for concerns to be identified early. The ability to detect issues before they escalate leads to more timely and effective intervention, often reducing the need for more intensive treatment later on.
Furthermore, PNPs are skilled at initiating sensitive conversations with both children and their parents. They help families understand the nature of emotional and behavioral health, reducing stigma and encouraging open dialogue. When specialized mental health care is needed, PNPs can make appropriate referrals while continuing to provide support and follow-up within the family clinic. This creates a more integrated and responsive care pathway for young patients.
Supporting Chronic Disease Management in Children
Children with chronic health conditions such as asthma, Type 1 diabetes, and epilepsy require consistent monitoring and management to avoid complications. Pediatric Nurse Practitioners play a key role in this aspect of care, particularly in family practice settings where long-term relationships with patients are central to success. Their specialized training equips them to manage chronic conditions with precision and compassion.
PNPs work closely with families to develop individualized care plans that include medication management, lifestyle modifications, and regular monitoring. They also spend time educating parents and children about recognizing symptoms, avoiding triggers, and adhering to treatment regimens. This proactive approach ensures that families are not only informed but also empowered to participate actively in their child’s health management.
Their involvement in chronic care also reduces the burden on emergency services and specialist referrals. By providing consistent, comprehensive care within the clinic, PNPs help minimize disruptions to the child’s daily life. They become a constant presence in the care journey, helping to navigate both the medical and emotional aspects of managing a long-term condition. This kind of support system is invaluable for families facing the stress and uncertainty of chronic illness.
Improving Health Equity and Access to Care
Health disparities continue to affect millions of children across the country, particularly those from low-income or marginalized communities. Pediatric Nurse Practitioners are often at the front lines of addressing these disparities through accessible, inclusive care delivered within family practice clinics. Their presence ensures that even children without access to large medical centers can receive competent and compassionate care.
Family clinics that employ PNPs are better equipped to reach underserved populations. These practitioners often take on roles that go beyond clinical duties, acting as advocates for vulnerable families. Whether it’s helping a parent understand how to apply for Medicaid or connecting them with community resources, PNPs serve as a bridge between the medical system and the everyday lives of their patients.
Cultural competence and sensitivity are also hallmarks of effective pediatric care, and PNPs receive training to understand and respect diverse backgrounds. They adapt their communication styles, health education, and care strategies to meet the unique needs of each family. By promoting health equity from within the family practice setting, PNPs help build a more just and effective healthcare system that serves all children fairly.
A Strategic Investment for Family Practices
For family practice clinics, bringing a Pediatric Nurse Practitioner on board is not just a staffing choice, it is a strategic investment in the clinic’s long-term viability and patient satisfaction. PNPs enhance the clinic’s ability to offer full-spectrum care, allowing families to receive medical attention for both children and adults in one place. This streamlines operations and increases patient loyalty.
Financially, the inclusion of a PNP makes sense. Their compensation typically falls below that of a pediatrician, yet they are fully capable of managing a broad scope of pediatric care. Additionally, their services are reimbursable through most insurance plans, making them a cost-effective solution for expanding clinical capabilities without overextending resources. This operational efficiency is particularly valuable in today’s competitive healthcare environment.
From a reputational standpoint, offering in-house pediatric expertise strengthens the clinic’s standing within the community. Families are more likely to choose and stay with practices that demonstrate a genuine commitment to comprehensive, quality care for every member of the household. As healthcare continues to evolve, clinics that invest in pediatric nurse practitioners position themselves as leaders in delivering truly family-centered care.
Also Read: Nurse Practitioners: Your Roadmap to Building a Private Practice